Digital healthcare technology has fundamentally transformed the landscape of clinical trials, fostering a more patient-centered approach by enabling real-world data collection outside the traditional clinical setting. This shift, characterized by a significant increase in the utilization of digital health technologies (DHTs) such as wearables for personal data collection at home, has seen the relative frequency of clinical trials employing DHTs soar from 0.7% in 2010 to an impressive 11.4% by 2020. Moreover, the advent of digital technology has streamlined the execution of decentralized and hybrid clinical trials on a global scale, marking a pivotal evolution in the field.
Integrating technology in clinical trials, from artificial intelligence in diagnostic devices to leveraging real-world data for study recruitment, introduces several advantages. These include heightened transparency, augmented collaboration, and reduced burdens on patients and study sites, which are pivotal for large-scale, international studies. Furthermore, healthcare technology innovations align with the principle of patient focus, significantly enhancing efficiency and productivity within clinical trials. With an eye on the future, this article discusses the role of wearable devices, telemedicine, remote monitoring, AI, and big data analytics, framing a comprehensive view of how digital healthcare technology redefines clinical trials.
Evolution of Technology in Clinical Trials
The COVID-19 pandemic has undeniably served as a catalyst for healthcare technology and innovation within clinical research, particularly highlighting the successful implementation and uptake of decentralized and hybrid clinical trials globally. This significant shift towards digitalization has enabled clinical trials to be conducted virtually, eliminating the need for in-person interactions. The advancements in digital healthcare technology, including the integration of synthetic biology, virtual reality, and the Internet of Things, are poised to disrupt the traditional drug development enterprise, offering a glimpse into the future of clinical trials.
Innovations and Their Impact:
- Synthetic Biology, Virtual Reality, and IoT: These exponential technologies are reshaping the landscape of drug development, offering novel approaches to clinical trials.
- Direct-to-Patient Research: This approach focuses on building patient communities, enhancing engagement, and facilitating continuous measurement of activity and behavior. It allows for the collection of precise and frequent information at a relatively low cost.
- Digital Signatures and Continuous Monitoring Enable the characterization of different populations’ behavior, improving the efficiency and productivity of clinical trials, particularly in neuroscience.
Integrating digital technologies into clinical trials over the past five years has not only improved the design and implementation of these studies but has also addressed several longstanding challenges. Mobile communications and wearable technology advancements have played a pivotal role in enhancing patient recruitment, especially in underserved communities, and in automating data monitoring to collect a wealth of data efficiently. Central data hubs facilitate data accessibility across multiple locations, significantly improving the analysis of big data and the overall patient experience.

Challenges and Solutions:
- Privacy and Confidentiality: Maintaining participant privacy while ensuring data accuracy remains a challenge. However, many Institutional Review Boards (IRBs) and regulatory agencies have issued guidance to navigate these concerns.
- Infrastructure and Resources: Ensuring access to adequate infrastructure, resources, and staff expertise is crucial. Conducting feasibility studies before main trials can help understand technology use preferences in target populations.
- Engagement and Retention: Keeping participants engaged and increasing retention are ongoing challenges. Leveraging social media for outreach and utilizing mobile devices and wearable technology for data collection are effective strategies to address these issues.
This healthcare technology evolution underscores the sector’s gradual yet increasing demand for breakthroughs, driven by rising costs, higher rates of trial failures, and a shift towards patient-centric trials. The integration of wearable technology, AI, big data analytics, synthetic biology, telemedicine, and mobile apps is not only fostering faster recruitment and better participant retention but is also paving the way for a more patient-centric approach through remote patient monitoring and decentralization of trials.
The Role of Wearable Devices
Wearable devices such as smartwatches and fitness trackers have revolutionized the landscape of healthcare technology and clinical trials, offering seamless integration into participants’ daily lives while providing invaluable data. The widespread adoption of these devices has been driven by their ability to measure physiological changes in real-time, including: accurately
- Heart Rate
- Glucose Levels
- Blood Pressure
This real-time monitoring allows for continuous observation of a patient’s health status, enabling prompt intervention should potential problems arise. Moreover, the objective data harvested from wearables have proven to be good indicators of depression and other psychiatric conditions, showcasing the broad potential of these devices in the realm of mental health.
The challenges associated with wearable devices in clinical trials primarily revolve around data management. The sheer volume of data generated necessitates advanced analytical frameworks to differentiate meaningful signals from noise. Despite these challenges, the integration of wearable medical technology and telehealth holds vast potential for the future of healthcare technology and clinical trials. Key advantages include:
- Enhanced Data Collection: Wearable devices collect data 24/7 in natural settings, providing a more accurate picture of a patient’s health than traditional methods.
- Objective Measures: In later stages of clinical development, sensors offer objective measures of outcomes traditionally reported subjectively, such as pain and fatigue.
- Early Safety Signals: Wearables can identify early safety issues and inform dose adjustments, potentially leading to the discontinuation of development for certain drug candidates.
The role of wearable devices in clinical trials extends beyond data collection, fundamentally changing the design and execution of studies. They offer researchers a real-world view of a patient’s response to treatment, facilitate earlier decision-making through access to near-continuous real-time data, and allow for more accurate intervention triggers. Furthermore, wearable devices can significantly improve subject retention by delivering prompts and sharing information to encourage active participation. This reduces the costs associated with clinic visits and enhances the effectiveness of trials through lower clinical site time and personnel needs.
In summary, wearable devices in clinical trials and healthcare technology represent a paradigm shift towards more patient-centric, efficient, and effective research methodologies. They enable:
- Improved Patient Phenotyping: Through more insightful data, including actigraphy and electrocardiography.
- Increased Efficiency: By reducing the need for manual data records and clinical visits.
- Enhanced Patient Participation: By offering patients access to their health metrics and reducing the burden of clinical setting visits.
As the digital age continues to unfold, the integration of wearable devices in clinical trials will undoubtedly play a pivotal role in shaping the future of healthcare research, offering promising avenues for innovation and improved patient outcomes.
Telemedicine and Remote Monitoring
Telemedicine and mobile communications have significantly expanded the reach and inclusivity of clinical trials and healthcare technology, introducing a patient-centric model that leverages digital healthcare technology for comprehensive remote monitoring and efficient data collection. The integration of medical technologies facilitates real-time physiological monitoring and direct communication between patients and healthcare providers, transforming clinical trials into more accessible and engaging experiences for participants across the globe. The following key points underscore this shift towards hybrid or decentralized trials powered by healthcare technology:
- Broadening Patient Demographics: Telemedicine opens clinical trials to a wider demographic, enabling participation from remote or underserved communities, thereby enhancing the diversity and representativeness of clinical research.
- Enhanced Patient and Family Participation: Telemedicine’s convenience encourages greater involvement from patients and their families, fostering a supportive environment for participants.
- Efficient Data Collection and Feedback: Tools such as wearable devices, mobile apps, and electronic patient-reported outcomes (ePRO) facilitate the capture of patient data in real time and from remote locations, streamlining the data collection and analysis process.
The advent of the COVID-19 pandemic has spotlighted remote monitoring as a critical component of clinical trials and an integral part of healthcare technology, driving innovation in remote site access and monitoring tools. These advancements reduce the operational costs of clinical trials and enhance their efficiency and effectiveness by providing a more thorough understanding of patient reactions and conditions. A study conducted at the Bégin Military Teaching Hospital highlighted the effectiveness of telemonitoring platforms, reporting high levels of patient compliance (76%) and satisfaction (95%). However, it also noted that telemedicine cannot completely replace the need for in-person care, as evidenced by unscheduled hospitalizations during the study period.

Remote monitoring tools offer several advantages, including:
- Cost Reduction and Efficiency Improvement: By eliminating the need for travel, telemedicine and remote monitoring significantly lower costs and improve the efficiency of clinical trials.
- Safety and Data Quality: Remote patient monitoring (RPM) systems equipped with real-time alert capabilities enhance patient safety and data accuracy, reducing the risk of infection and improving the quality of collected data.
- Innovative Protocol Designs: The critical role of remote monitoring in decentralized trials supports more innovative and efficient study designs, emphasizing the need for digital tools in remote data acquisition to be fit-for-purpose, accurate, usable, and validated.
Integrating telemedicine and remote monitoring in clinical trials represents a pivotal shift towards more innovative, efficient, and patient-centric research methodologies. By leveraging digital healthcare technology, clinical trials can achieve greater inclusivity, enhance participant engagement, and improve research outcomes’ overall quality and reliability.
AI and Big Data Analytics
In the rapidly evolving landscape of clinical trials, AI and big data analytics are playing a transformative role, streamlining processes and enhancing the efficiency of research and development. Integrating these advancements is not just an innovation but a necessity, addressing critical challenges and unlocking new opportunities in the realm of healthcare technology.
Also Read: Precision Medicine: How Big Data and Genomics are Revolutionizing Treatment?
AI’s Role in Clinical Trials:
- Recruitment and Retention: AI algorithms analyze vast patient data from medical records to identify optimal candidates, addressing traditional recruitment and retention challenges.
- Digital Twins: Creating virtual patients or digital twins through AI and machine learning offers a glimpse into future clinical trials where external control arms could replace placebos.
- Data Management: AI automates the entire trial lifecycle, from patient recruitment to enrollment and from frequent monitoring to ensuring medical adherence and retention. This automation extends to intelligent data interpretation, feeding downstream systems, and automatically fulfilling analysis report requirements.
Big Data Analytics in Clinical Trials:
- Volume, Velocity, and Variety: Big data in clinical trials encompass various data sources, including EHRs, genetic sequencing, and wearable device data. Its three Vs—volume, Velocity, and Variety—characterize the massive, fast-moving, and diverse nature of data sets that researchers now have at their disposal.
- Risk-Based Monitoring (RBM): RBM utilizes increased connectivity and advances in data analytics to streamline and optimize error detection, a strategic approach that significantly enhances trial efficiency.
The Future of Clinical Trials with AI and ML:
- Drug Discovery and Development: AI and ML are set to revolutionize drug discovery and development processes by improving image interpretation, streamlining EMR data, and enhancing trial workflows.
- Optimizing Drug Development: Machine learning algorithms not only predict cancer risk by identifying patterns within large datasets but also streamline drug target identification and molecule generation, optimizing the drug development process within the constraints of targeted biological systems.
The integration of AI and big data analytics into clinical trials signifies a monumental shift towards more efficient, patient-centered, and innovative research methodologies. By leveraging these technologies, the future of clinical trials promises accelerated medical breakthroughs, reduced costs, and a more profound understanding of diseases and treatments. As the digital age advances, the seamless synergy of AI, machine learning, and big data analytics will continue to redefine the boundaries of what is possible in clinical research, setting new benchmarks for efficiency, effectiveness, and patient-centricity in the process.
Also Read: Robotics in Healthcare.

Navigating Challenges and Future Perspectives
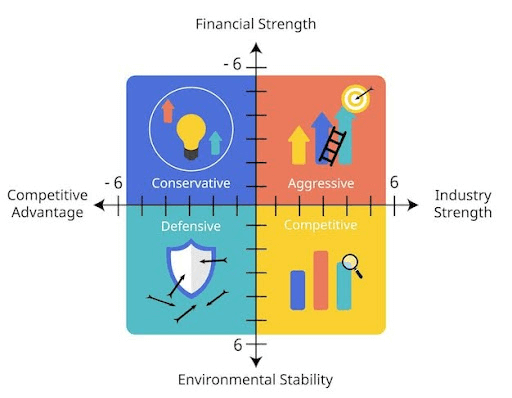
Navigating the complex landscape of digital healthcare technology in clinical trials involves addressing multifaceted challenges while embracing future perspectives to enhance research methodologies and patient outcomes. The integration of advanced technologies raises both opportunities and obstacles that require strategic solutions and innovative approaches.
Challenges in Implementing Digital Healthcare Technology:
- Health Inequalities and Technology Poverty: A significant concern is that the incorporation of more healthcare technology in clinical trials could exacerbate health inequalities, necessitating an individualized approach to trial recruitment and mechanics to ensure inclusivity.
- Regulatory and Operational Concerns: As healthcare technology advances, monitoring bodies introduce regulatory and operational challenges that must be navigated carefully to maintain compliance and ensure the integrity of trial data.
- Data Security and Privacy: Implementing decentralized clinical trials (DCTs) involves ensuring robust data security and privacy measures to protect sensitive patient information, a challenge accentuated by the vast amounts of data generated.
Strategies for Overcoming Challenges:
- Adopting an Individualized Approach: Tailoring trial recruitment and mechanisms to address health inequalities and technology poverty, ensuring trials are accessible and equitable.
- Navigating Regulatory Landscapes: Staying abreast of evolving regulatory guidelines and engaging with regulatory bodies early in the trial design process can mitigate concerns around healthcare technology and streamline approvals.
- Enhancing Data Security Measures: Implementing stringent data security protocols, including encryption, secure data transmission, and compliance with regulations such as HIPAA, is crucial for safeguarding patient information.
Future Perspectives in Clinical Trials:
- Increased Patient Engagement and Decentralization: Future trials are expected to be more decentralized and virtualized, incorporating digitalized endpoints for globally harmonized, standardized real-world tracking of patient experiences. This shift promises enhanced patient engagement, reduced patient burden, and improved data quality.
- Collaborative Efforts for Efficiency: Collaborative efforts among academic institutions, patients, sponsors, regulatory organizations, and CROs are anticipated to improve the research landscape, making trials more time and cost-effective.
- Innovation through Exponential Technologies: Technologies such as synthetic biology, virtual reality, and the Internet of Things are poised to disrupt drug development further, offering novel approaches to clinical trials that could accelerate drug development and improve patient outcomes.
By addressing the challenges head-on and leveraging the potential of digital healthcare technology, the future of clinical trials looks promising, with the potential to transform patient care and accelerate medical breakthroughs.
Conclusion
Throughout this article, we’ve witnessed how digital healthcare technology is revolutionizing the field of clinical trials, from enhancing patient participation with wearable devices to leveraging AI and big data for more efficient trial processes. The significant shift towards digitalization, emphasized by the declining traditional face-to-face clinical settings in favor of decentralized and hybrid models, underscores a transformative era in clinical research. This evolution not only addresses the historical challenges of engagement and data collection but also opens up a more inclusive and comprehensive approach to patient care and medical discovery.
Looking ahead, the persistent integration of innovative technologies in clinical trials signals a promising horizon for both research methodologies and patient outcomes. Embracing the digital age, the clinical trial landscape is set to become more patient-centric, efficient, and effective, facilitating a bridge between pioneering research and real-world healthcare applications. As we continue to navigate the complexities and potentials of digital healthcare technology, the commitment to improving patient experiences and outcomes remains paramount, heralding a new epoch of medical research and development.
FAQs
What effects does digital healthcare technology have on patient care?
Digital healthcare technology grants patients access to their health information, including medical records, test results, and tools for managing their own health. This empowers patients to actively participate in making informed decisions about their care in collaboration with their healthcare providers.
How do clinical trials contribute to advancements in medical technology?
Clinical trials play a crucial role in the discovery of new treatments for diseases and in the development of novel methods for detection, diagnosis, and prevention. They provide researchers with essential information about what is effective in humans, which cannot be obtained through laboratory experiments or animal studies.
In what ways has digital technology transformed healthcare?
Digital technology has revolutionized healthcare by speeding up communication and facilitating the transition from paper to electronic medical records. This shift has streamlined record-keeping and made it easier for patients to transfer their medical information when changing healthcare providers.
What are the recent technological innovations in conducting clinical trials?
Recent technological innovations in clinical trials include the adoption of telemedicine, remote patient monitoring, and electronic consent. These technologies enable patients to participate in clinical trials from their homes, reducing the necessity for frequent visits to the trial sites and enhancing overall convenience.
 1-800-805-5783
1-800-805-5783